TOLL FREE:
1-866-611-2665
Home HOW CAN X-RAY HELP DIAGNOSE ARTHRITIS?
According to the Arthritis Society of Canada, one in five Canadians live with arthritis every day. The term arthritis applies to over 100 diseases, which most often cause inflammation in the joints. Inflammation is redness and swelling which can cause pain and stiffness in the joints.
There are two main categories of arthritis conditions:
For both categories of arthritis, the symptoms can include the following:
OA usually progresses slowly over months or years and early symptoms tend to come and go. It commonly affects the knees, hips, first toes, wrists, thumbs, fingers, and spine. As damage progresses, symptoms can become more constant, occurring at rest and disturbing sleep.
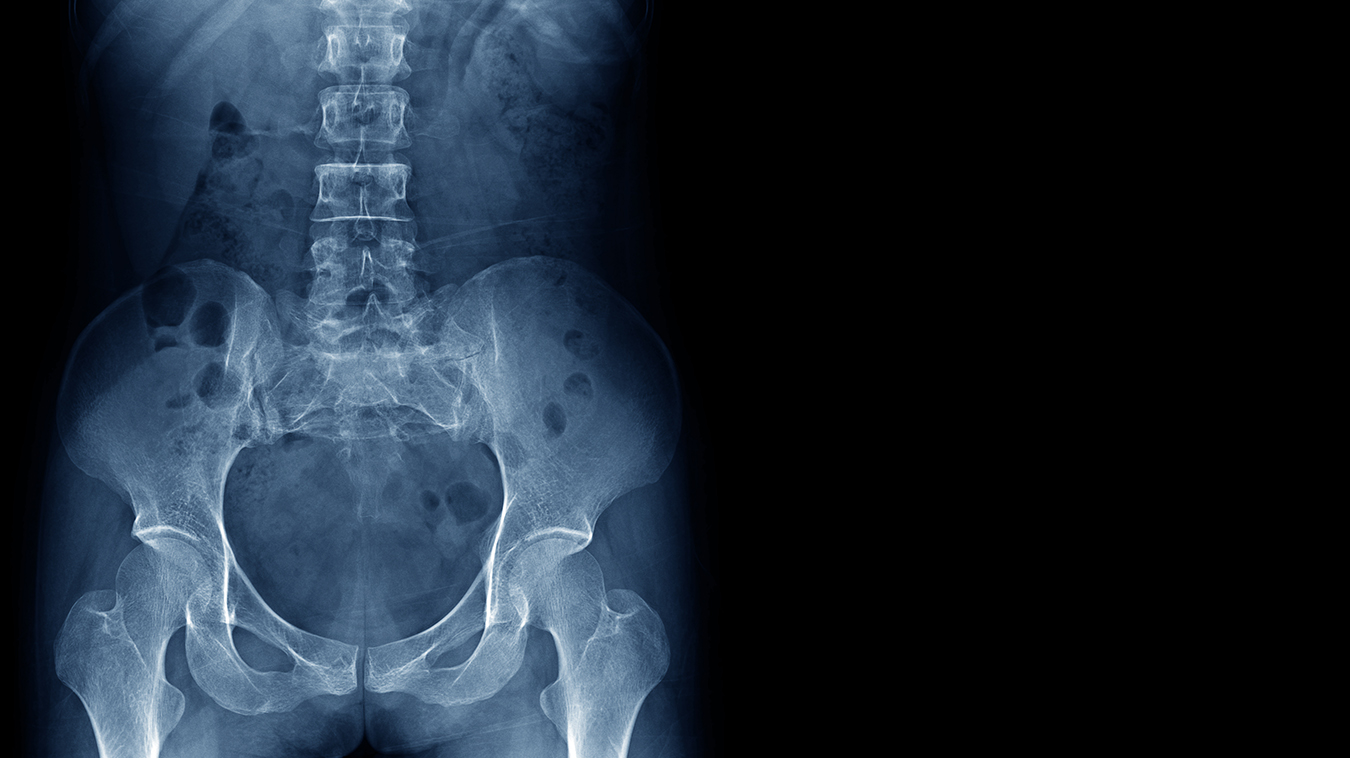
Osteoarthritis is usually diagnosed through a clinical assessment based on your symptoms and a physical examination. X-ray may be ordered to confirm the diagnosis and establish the severity of your OA. For suspected inflammatory arthritis, you will be referred to a rheumatologist, but X-ray may also be ordered to look for signs of OA or to monitor the progression of the disease.
X-ray is often the first step for imaging to investigate arthritis because its inexpensive and readily accessible. On the X-ray image, the radiologist will look for:
Magnetic resonance imaging (MRI) may also be ordered when investigating arthritis. MRI can help provide information about cartilage, tendons, and other structures in the joint, as well as showing the presence of swelling caused by too much fluid in your tissue (edema).
For osteoarthritis, treatment options can vary depending on the stage of progression of the disease. Bracing and wraps to ensure joint stability may help at any stage. In the early stages, weight loss and exercise may be recommended to slow the progression of the disease, and oral nonsteriodal anti-inflammatory drugs (NSAIDs), like ibuprofen or naproxen, may be ordered to help relieve pain and inflammation. Other options include:
For inflammatory arthritis conditions, some of the initial treatment options are similar to those for OA, such as exercise and weight loss or diet changes. Other treatments can include anti-rheumatic and anti-inflammatory medication, as well as cortiocosteriod injections.
Arthritis conditions are chronic (long-term) and, although there is no cure, treatment can help reduce your symptoms and make it possible for you to lead a full and active life. Studies suggest treatment in early stages of the disease is the most effective way to prevent progression. In most cases, you can manage mild to moderate arthritis symptoms for many years with a treatment plan. It’s also important to thoroughly discuss all your options with your health care practitioner, especially in the later stages of the disease.
For more information on pain management injections, please speak to your health care practitioner.
REFERENCES
Arthritis Society Canada (2023) “What is arthritis?” www.arthritis.ca. Accessed July 12, 2023.
Bennington-Castro, J. (2023) “What Is Osteoarthritis? Symptoms, Causes, Diagnosis, Treatment, and Prevention.” www.everyday.health. Accessed July 12, 2023.
Frank, J. (2021) “Rheumatoid Arthritis (RA) Diagnosis.” www.arthritis-health.com. Accessed July 12, 2023.
Holland, K. (2023) “Stages of Osteoarthritis (OA) of the Knee.” www.healthline.com. Accessed July 12, 2023.
Johns Hopkins Arthritis Centre (2023) “Osteoarthritis: Signs and Symptoms.” www.hopkinsarthritis.org. Accessed July 12, 2023.
Our Refresh newsletter delivers the latest medical news, expert insights, and practical tips straight to your inbox, empowering you with knowledge to enhance patient care and stay informed.
By subscribing to our newsletter you understand and accept that we may share your information with vendors or other third parties who perform services on our behalf. The personal information collected may be stored, processed, and transferred to a country or region outside of Quebec.
Please read our privacy policy for more details.