TOLL FREE:
1-866-611-2665
Home WHAT’S THE DIFFERENCE BETWEEN MAMMOGRAPHY AND BREAST ULTRASOUND?
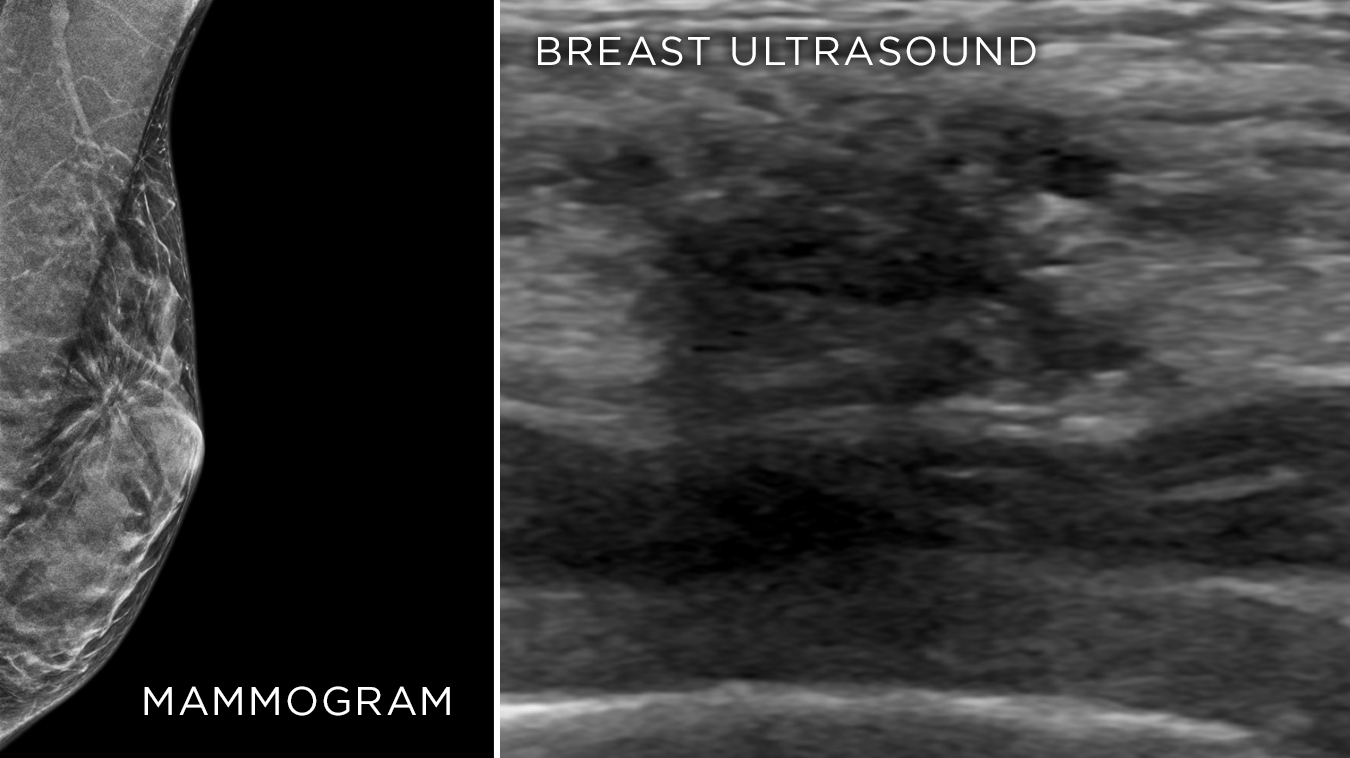
Mammography and breast ultrasound use different types of imaging technology and are often ordered together to help provide a comprehensive look at breast tissue.
Mammography is a type of X-ray exam that takes an image of the inside of the breasts – called a mammogram. It provides a detailed look at the internal structure of breast tissue and can reveal changes that are too small to feel. Mammograms provide a very good picture of breast tissue, but sometimes the images can be complex.
A breast ultrasound uses high-frequency sound waves to help determine the composition of a lump or area of concern, distinguishing between a cyst, fibroglandular tissue, and a solid mass. The sound waves travel into the breast until they hit a boundary between tissues, such as fluid and soft tissue, or soft tissue and bone. At these boundaries some of the sound waves are reflected back to the probe, while others travel farther until they reach another boundary and are reflected back. Since the pitch, direction, and distance sound waves travel differ depending on the boundary they run into, a computer can interpret this information as a two-dimensional image on a screen and provide information about the area of concern.
By combining these two imaging types, radiologists can get a clearer picture of both the look and composition of the area of concern. This is especially important for women with dense breast tissue.
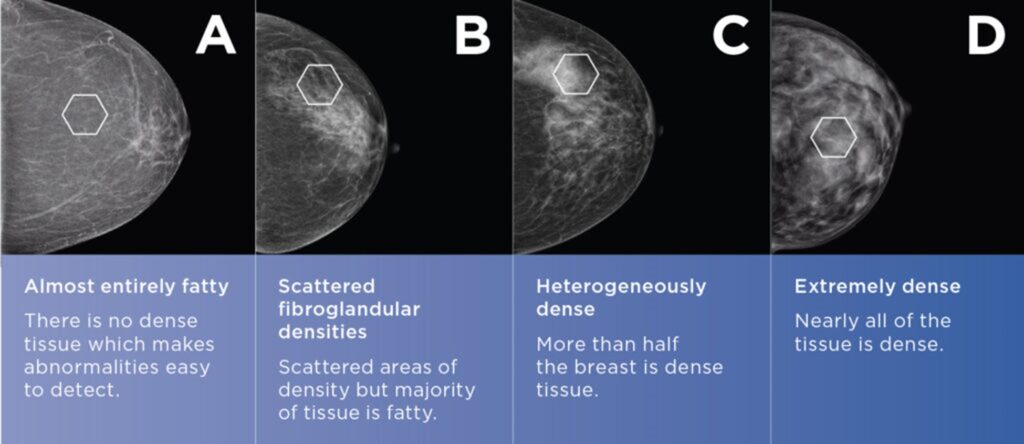
Your breasts are made up of different types of tissue: fibroglandular and connective tissue, and fat. At Mayfair Diagnostics mammography clinics our equipment has software that helps determine your breast density – a measure of the proportion of fatty (not dense) versus connective and fibroglandular (dense) tissue that make up your breast. Breast density does NOT have to do with the size, look, or feel of your breast.
For women, breast density is the most prevalent risk factor for breast cancer. Sometimes a breast ultrasound may be performed along with your screening mammogram, if you meet the criteria below:
Breast density is scored from A to D:
Mammography is the gold standard for breast cancer screening; it’s the best way to detect cancer in its early, most treatable stage. Unlike mammography, breast ultrasound in isolation is NOT authorized by the College of Physicians and Surgeons of Alberta as a screening tool for early detection of breast cancer. This applies to both handheld and automated breast ultrasound.
Screening describes routine imaging that is ordered without specific symptoms or concerns, such as annual mammograms. It can be used to help detect diseases before they cause symptoms and while they can still be successfully treated.
Breast ultrasound is considered a diagnostic tool. This means that it’s ordered to investigate a specific concern, such as:
Having regular screening mammograms makes it easier to compare images and see changes that are too small for you or your doctor to feel. These exams can be requested for women 40 and over when there are no symptoms, as part of a breast screening program. The Alberta Health Insurance Plan covers one screening mammogram per year for women, starting at age 40.
Breast cancer will affect one in eight women in Canada, but if you find it early, there is less chance of recurrence and an increased chance that it has not spread to the lymph nodes, so the odds are better you will survive it. Thanks to preventative screening more women are surviving a breast cancer diagnosis. In 2017, 89% of women diagnosed with breast cancer were still alive after five years.
During a screening mammogram, four images are taken. Occasionally you may be asked to return for additional breast imaging, such as a diagnostic mammogram and/or diagnostic breast ultrasound. This is done to get a more detailed look at any areas of concern and ensure you have received a complete breast exam.
Women with the following risk factors are considered high risk and may need to start having regular mammograms earlier and more frequently, and supplemental diagnostic breast ultrasound may also be ordered regularly.
Please note that having a family history of breast cancer does not mean that you WILL develop breast cancer; it simply increases your risk. Many women who develop breast cancer do not have a family history of the disease, which is why screening is important for all women, regardless of family history.
Mayfair Diagnostics has 14 locations which offer mammography exams, and except for our Coventry Hills all of them use the Senographe Pristina mammography system – which helps provide a more comfortable mammogram. Visit our breast imaging page for more information.
REFERENCES
American Cancer Society (2024) “Key Statistics for Breast Cancer.” www.cancer.org. Accessed February 15, 2024.
Canadian Cancer Society (2024) “Risks for breast cancer.” cancer.ca. Accessed February 15, 2024.
Canadian Cancer Society (2023) “Breast cancer statistics.” cancer.ca. Accessed February 15, 2024.
Engmann, N.J., et al. (2017) “Population-Attributable Risk Proportion of Clinical Risk Factors for Breast Cancer.” JAMA Oncology. 2017; 3(9) 1228-36.
Alberta Health Services (2021) “Breast Screening.” screeningforlife.ca. Accessed February 15, 2024.
Our Refresh newsletter delivers the latest medical news, expert insights, and practical tips straight to your inbox, empowering you with knowledge to enhance patient care and stay informed.
By subscribing to our newsletter you understand and accept that we may share your information with vendors or other third parties who perform services on our behalf. The personal information collected may be stored, processed, and transferred to a country or region outside of Quebec.
Please read our privacy policy for more details.